Imagine spending years being told something is fundamentally wrong with you — that your anxiety, your anger, your difficulty trusting people, your trouble sleeping — are symptoms of a disordered brain. Now imagine a clinician sitting across from you (or, increasingly, on the other side of a secure video screen) who asks instead: “What happened to you?” For many people, that single shift in framing is the moment real healing begins. This is trauma-informed care.Trauma-informed care (TIC) is the foundation and one of the most significant evolutions in modern mental health practice. It is not a single therapy or a technique you can master in a weekend workshop. It is a way of seeing people: their struggles, their defenses, their seemingly “difficult” behaviors, through the lens of what they have survived rather than what they lack. And the research backing it up grows stronger every year. Critically, TIC is not a specific treatment — it is an overarching philosophy applied across organizations, policies, clinical interactions, and even the physical environments where care is delivered. It applies to healthcare, education, social services, and crisis response. Its goal is simple but profound: create conditions where healing and growth are actually possible.
Critically, TIC is not a specific treatment — it is an overarching philosophy applied across organizations, policies, clinical interactions, and even the physical environments where care is delivered. It applies to healthcare, education, social services, and crisis response. Its goal is simple but profound: create conditions where healing and growth are actually possible.
 If you recognized yourself in that list, you’re not alone — and you’re not broken. The path forward starts with a conversation. One that begins, for once, with the right question.
If you recognized yourself in that list, you’re not alone — and you’re not broken. The path forward starts with a conversation. One that begins, for once, with the right question.
What Exactly Is Trauma-Informed Care?
Trauma-informed care is a strengths-based framework grounded in an understanding of the widespread impact of trauma — and what it does to the body, brain, behavior, and relationships long after the original event has passed. Rather than treating mental health symptoms as isolated problems to be extinguished, TIC recognizes them as meaningful responses to overwhelming life experiences.The Substance Abuse and Mental Health Services Administration (SAMHSA) identifies six core principles that define a trauma-informed approach:The Six Core Principles of Trauma-Informed Care
- Safety — Ensuring physical and emotional security in every interaction and environment
- Trustworthiness & Transparency — Building relationships through honesty, consistency, and clear communication
- Peer Support — Integrating lived experience into the delivery of care
- Collaboration & Mutuality — Sharing power and decision-making between provider and patient
- Empowerment, Voice & Choice — Validating strengths and supporting self-determination
- Cultural, Historical & Gender Responsiveness — Addressing biases and systemic inequities that shape trauma
“Rather than asking ‘What’s wrong with you?’ trauma-informed care shifts the focus to ‘What happened to you?’ — recognizing that trauma shapes brain function, behavior, relationships, and health outcomes in ways that demand a fundamentally different clinical response.”— Core principle of Trauma-Informed Care frameworks
Why This Approach Matters: What the Science Says
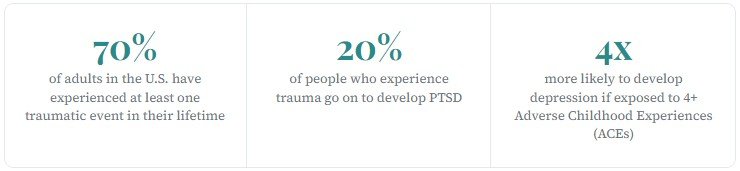
The evidence base for trauma-informed care has been building for decades, anchored by the landmark CDC–Kaiser Adverse Childhood Experiences (ACE) Study, which found that childhood adversity — abuse, neglect, household dysfunction — is directly linked to a dramatically increased risk of mental illness, chronic disease, substance abuse, and even early death in adulthood. The more ACEs a person experiences, the steeper the risk curve becomes.But the science doesn’t stop at childhood. Research consistently shows that people with histories of trauma are more likely to be hospitalized, more likely to be prescribed higher doses of medication, and more likely to engage in self-harm — not because of a character flaw, but because their nervous systems learned to survive in environments that weren’t safe. Those survival strategies, hardwired over years, don’t simply disappear when the danger does.A landmark 2025 study published in Frontiers in Psychology examined what happened when a major NHS inpatient mental health unit introduced trauma-informed practices — including staff training and structured team formulations — over a six-year period. The quantitative outcomes were striking: significant reductions in self-harm incidents, seclusion, and the use of physical restraint. But perhaps even more compelling were the qualitative findings.Staff reported a fundamental shift in how they understood patient behavior. Rather than seeing agitation and aggression as symptoms to manage, they began seeing them as threat responses — intelligible attempts to survive past harm. One staff member described the transformation during team formulation meetings: participants would begin by expressing frustration with a patient, and by the end, after understanding the person’s history, the room’s emotional temperature had shifted entirely toward compassion. The research described this as a “shift in ideology” — from What’s wrong with you? to What happened to you? — and identified it as the single most important catalyst for all the measurable improvements that followed.Service users reported gaining new skills for managing their distress, feeling truly heard for the first time, and leaving with a deeper understanding of why they had struggled in the ways they had. Several compared this admission favorably to previous ones, noting that earlier hospitalizations had focused on medication and containment rather than understanding and skill-building.Trauma and the Brain: Understanding Why Symptoms Make Sense
One reason trauma-informed care is so transformative is that it aligns with what neuroscience has revealed about trauma’s effects on the brain. Traumatic experiences alter the structure and function of key brain regions — particularly the amygdala (the brain’s threat-detection center), the hippocampus (involved in memory and context), and the prefrontal cortex (responsible for rational thought and emotional regulation).When someone has experienced repeated trauma, especially in childhood, their nervous system essentially recalibrates itself for a world that is dangerous. Hypervigilance, emotional dysregulation, difficulty with trust, dissociation, avoidance — these are not character defects. They are adaptive responses that helped a person survive something genuinely threatening. A trauma-informed lens honors that history rather than pathologizing it.This biological understanding is why trauma-informed care pairs so effectively with evidence-based therapies. Cognitive Behavioral Therapy (CBT), for example, becomes far more effective when delivered within a framework that first establishes safety, trust, and collaboration — the prerequisites that trauma often disrupts. Similarly, approaches like EMDR, DBT, and somatic therapies all build on these same foundational principles.
At East Coast Telepsychiatry, we provide trauma-informed care through our online psychiatry services, designed for those seeking virtual mental health care across the region. Our trauma-informed telepsychiatry approach combines science-backed compassion with telehealth psychiatric treatment to support patients through every stage of recovery.
What Trauma-Informed Care Looks Like in Practice
Trauma-informed care isn’t an abstract philosophy — it shows up in concrete, specific ways in every clinical interaction. Here’s what it can look like when a provider truly embraces this approach:1. The First Conversation Is Different
A trauma-informed intake doesn’t begin with a symptom checklist. It begins with curiosity about your story. Rather than jumping to diagnosis, a trauma-informed clinician takes time to understand your history, your context, and what brought you to this moment. They ask with care — and they listen with intention.2. Your Reactions Are Treated as Meaningful, Not Problematic
If you shut down in sessions, become tearful without warning, or feel sudden distrust toward your provider, a trauma-informed clinician doesn’t interpret these as resistance or non-compliance. They understand that these are nervous system responses with real histories — and they work with you to understand and navigate them.3. Safety and Stabilization Come First
Deep trauma processing is only possible once you have the skills and internal resources to handle difficult material without becoming overwhelmed. Trauma-informed care prioritizes this foundation — teaching grounding techniques, emotional regulation strategies, mindfulness, and self-compassion before diving into traumatic memories.4. You Are a Partner, Not a Patient
Collaboration is a cornerstone of TIC. Your goals, your pace, your comfort level — these shape the treatment plan. Nothing is done to you; everything is done with you. This is not just a philosophical nicety. For survivors of trauma — especially those whose experiences involved powerlessness — having genuine agency in their care is itself therapeutic.5. Cultural and Systemic Context Is Acknowledged
Trauma doesn’t happen in a vacuum. Racism, poverty, discrimination, historical injustice, gender-based violence — these are real forces that shape who gets traumatized and how deeply. Trauma-informed care refuses to treat individuals as if their struggles are purely personal, divorced from the systems and structures that surround them.“Trauma-informed care is not about asking whether someone has experienced trauma — it’s about assuming they may have, and proceeding with the kind of care that would help anyone who has.”
Trauma-Informed Telepsychiatry: Healing on Your Terms
One of the most powerful — and often underappreciated — aspects of telepsychiatry is how naturally it aligns with trauma-informed principles. For many trauma survivors, the barriers to in-person mental health care are significant and deeply personal: leaving home feels unsafe, waiting rooms are overwhelming, sitting in a clinical office triggers unwanted memories, or the simple logistics of transportation and scheduling feel insurmountable in the weight of depression or PTSD.East Coast Telepsychiatry delivers care in a way that addresses these barriers directly. When you connect with a provider from your own home — in a space you’ve chosen, in a chair you trust, with your cat on your lap if that helps — you arrive at the session with something trauma survivors rarely get to have: control. That sense of control isn’t incidental. It’s a clinically meaningful ingredient in the healing process.Our board-certified providers are experienced in treating Trauma-related and co-occurring conditions — including PTSD, complex trauma, anxiety disorders, depression, and mood disorders — with approaches grounded in the same evidence-based, trauma-informed principles described throughout this article. Services are available across the East Coast, including New York, New Jersey, Maryland, Virginia, North Carolina, South Carolina, and Florida, with appointments conducted via secure, HIPAA-compliant video technology.For people who have been dismissed, misdiagnosed, or left feeling more broken by systems that were supposed to help them, finding care that actually sees you — that starts not with what’s wrong with you but with what happened to you — can be a turning point. That is what trauma-focused telepsychiatry offers: not just treatment, but the experience of being understood.
Whether you’re searching for affordable virtual psychiatry services near me or want to connect with licensed online psychiatrists East Coast, our team ensures you receive personalized, trauma-focused telepsychiatry designed to promote safety, empowerment, and healing from trauma and PTSD.
Is Trauma-Informed Care Right for You?
You don’t need a formal PTSD diagnosis to benefit from trauma-informed care. In fact, many people who carry the weight of trauma have never been given that label — and many wouldn’t recognize their experiences as “trauma” at all. If any of the following resonate with you, a trauma-informed approach may be worth exploring:Signs a Trauma-Informed Approach May Help
- You struggle with anxiety, hypervigilance, or feeling constantly “on edge”
- Relationships feel difficult — you pull away, or fear abandonment
- You experience emotional reactions that feel disproportionate and hard to explain
- You’ve felt like mental health treatment hasn’t worked, or like providers don’t truly understand you
- You experienced adversity, abuse, neglect, or significant loss in childhood or adulthood
- You avoid certain memories, places, or conversations without fully understanding why
- You feel a persistent sense of shame or the belief that something is fundamentally wrong with you
Ready to Experience Care That Starts With Your Story?
Our compassionate, board-certified providers deliver trauma-informed psychiatric care from the privacy and comfort of your home. Accepting most major insurance. Serving the East Coast.Schedule a Consultation →References & Further Reading
- Nikopaschos, F., et al. (2025). Trauma-Informed Care on mental health wards: staff and service user perspectives. Frontiers in Psychology, 16. doi:10.3389/fpsyg.2025.1578821
- SAMHSA. SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach. samhsa.gov
- Centers for Disease Control and Prevention. Adverse Childhood Experiences (ACEs). cdc.gov
- National Institute of Mental Health. Post-Traumatic Stress Disorder (PTSD). nimh.nih.gov
- Felitti, V.J., et al. (1998). Relationship of childhood abuse and household dysfunction to the leading causes of death in adults. American Journal of Preventive Medicine, 14(4).
